AI in Healthcare: Shaping the Future Responsibly
Published on: September 10, 2025

Annotation
- Table of Contents
- Introduction: The AI Revolution in Medicine
- What is AI in Healthcare? Deep Explanation
- Key Points: Core Insights from Industry Leaders
- Key Features and Capabilities of Healthcare AI
- Pros and Cons of Leveraging AI in Healthcare
- Frequently Asked Questions
- Related Questions: Exploring Further Implications
Table of Contents
- Introduction: The AI Revolution in Medicine
- What is AI in Healthcare? Deep Explanation
- Key Points: Core Insights from Industry Leaders
- Key Features and Capabilities of Healthcare AI
- Pros and Cons of Leveraging AI in Healthcare
- Frequently Asked Questions
- Related Questions: Exploring Further Implications
Introduction: The AI Revolution in Medicine
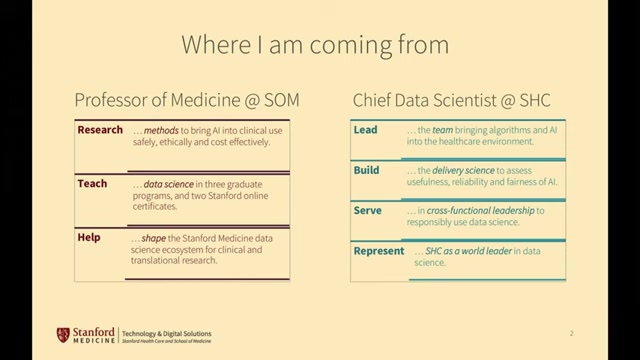
Artificial Intelligence is no longer a futuristic concept—it's actively reshaping the healthcare landscape with unprecedented speed and potential. As we stand at the precipice of what many are calling the fourth industrial revolution in medicine, understanding how to responsibly integrate AI into healthcare systems becomes paramount. This comprehensive guide explores the transformative power of AI in healthcare, drawing insights from leading experts like Nigam Shah, MBBS, PhD, Professor of Medicine at Stanford School of Medicine and Chief Data Scientist at Stanford Healthcare.
The integration of AI Productivity Tools into medical practice represents one of the most significant advancements in modern healthcare. From diagnostic algorithms that can detect diseases with superhuman accuracy to predictive models that anticipate patient deterioration hours before human clinicians, AI is revolutionizing how we approach patient care. However, this transformation comes with substantial responsibilities—ethical considerations, cost-effectiveness, and seamless clinical integration must be balanced against the tremendous potential benefits.
This article serves as a essential resource for healthcare professionals, technology enthusiasts, policymakers, and anyone interested in the future of medicine. We'll explore the current state of AI in healthcare, examine real-world applications, discuss implementation strategies, and address the critical questions surrounding responsible adoption. Whether you're a clinician looking to understand how AI can enhance your practice, a developer creating healthcare solutions, or simply someone fascinated by the intersection of technology and medicine, this guide provides valuable insights into one of the most important developments in modern healthcare.
What is AI in Healthcare? Deep Explanation
Artificial Intelligence in healthcare encompasses a broad range of technologies and applications designed to enhance medical decision-making, improve patient outcomes, and optimize healthcare delivery. At its core, healthcare AI involves using machine learning algorithms, natural language processing, computer vision, and other advanced computational techniques to analyze complex medical data, identify patterns, and generate insights that would be difficult or impossible for humans to discern unaided.
The foundation of healthcare AI lies in its ability to process and learn from vast amounts of data. Unlike traditional software that follows explicit programming instructions, AI systems improve their performance through exposure to data, essentially learning from experience. This capability makes AI particularly well-suited for healthcare applications, where patterns in patient data, medical images, and clinical notes can reveal critical insights about disease progression, treatment effectiveness, and individual patient needs.
One of the most significant aspects of healthcare AI is its relationship with data timelines. As Nigam Shah emphasizes, healthcare data exists as a "patient timeline object"—a dynamic sequence of events including medical visits, diagnoses, medications, lab results, and other clinical interactions. Unlike other industries where data might be static files, healthcare data is inherently temporal, with the relationship between events being critical for developing accurate and clinically useful algorithms. This temporal dimension presents both challenges and opportunities for AI development, requiring sophisticated approaches to data integration and model training.
The healthcare AI ecosystem includes various types of applications, from diagnostic tools that analyze medical images to predictive analytics systems that identify patients at risk of developing certain conditions. AI Chatbots are increasingly being used for patient triage and education, while natural language processing systems extract valuable information from unstructured clinical notes. The field also includes robotic process automation for administrative tasks and personalized treatment recommendation systems that consider individual patient characteristics and preferences.
As the field continues to evolve, we're seeing the emergence of increasingly sophisticated AI tools that can handle complex clinical tasks. These include systems that can integrate multiple data types (genomic, clinical, imaging, etc.) to provide comprehensive patient assessments, as well as AI-powered clinical decision support systems that help physicians make evidence-based treatment decisions. The ultimate goal is not to replace healthcare professionals but to augment their capabilities, providing them with powerful tools that enhance their ability to deliver high-quality, personalized care.
Key Points: Core Insights from Industry Leaders
The responsible adoption of AI in healthcare requires careful consideration of multiple factors beyond mere technological capability. According to Nigam Shah, who bridges the gap between academic research and clinical practice through his dual roles at Stanford School of Medicine and Stanford Health Care, the journey from concept to clinical implementation involves several critical steps: data, algorithms, policy, and finally action.
One of the most important insights from leading experts is that AI implementation must be driven by clinical need rather than technological possibility. It's easy to become enamored with advanced algorithms and impressive technical demonstrations, but the true measure of success is whether these tools actually improve patient outcomes, enhance efficiency, or reduce costs in real-world clinical settings. This requires close collaboration between technologists, clinicians, administrators, and patients throughout the development and implementation process.
Another crucial consideration is the fragmented nature of healthcare data. As Shah notes, Stanford HealthCare alone has data distributed across over 1,200 different IT systems. Assembling this fragmented data into coherent patient timelines is essential for building effective AI models, but it presents significant technical and logistical challenges. Furthermore, even when data can be assembled, complete datasets are rare—not all patients undergo the same tests or procedures, leading to gaps that must be addressed in AI development.
The importance of focusing on deployment affordability cannot be overstated. While innovative AI solutions are exciting, each application carries costs—not just financial, but also in terms of time, resources, and workflow disruption. Healthcare organizations must carefully consider whether they can afford to deploy and maintain AI solutions within their operational budgets, and whether the expected benefits justify these investments.
Finally, experts emphasize the need to balance AI integration with existing clinical workflows. AI should enhance, not disrupt, the work of healthcare professionals. This requires thoughtful design that considers how clinicians actually work, what information they need, and how AI tools can most effectively support their decision-making processes. Doctors need clear reasons to trust and use AI tools, which means demonstrating tangible benefits in terms of productivity, accuracy, or patient outcomes.
Key Features and Capabilities of Healthcare AI
Healthcare AI systems offer a wide range of capabilities that are transforming medical practice across multiple domains. One of the most significant features is diagnostic assistance, where AI algorithms can analyze medical images, lab results, and clinical data to help identify diseases and conditions. These systems often achieve accuracy levels comparable to or exceeding human experts, particularly in areas like radiology, pathology, and dermatology. For example, AI systems can detect subtle patterns in medical images that might be overlooked by human eyes, leading to earlier and more accurate diagnoses.
Predictive analytics represents another powerful capability of healthcare AI. By analyzing patterns in historical patient data, these systems can identify individuals at high risk of developing certain conditions, experiencing complications, or requiring hospitalization. This enables proactive interventions that can prevent adverse outcomes and improve patient health. Predictive models can also forecast disease progression, treatment response, and resource needs, helping healthcare organizations optimize their planning and resource allocation.
Natural language processing (NLP) capabilities allow AI systems to extract valuable information from unstructured clinical notes, research literature, and patient communications. This enables more comprehensive data analysis and can uncover insights that would be difficult to obtain through structured data alone. NLP-powered AI Writing Tools can also assist with clinical documentation, generating summaries, and maintaining accurate medical records, reducing administrative burden on healthcare professionals.
Personalized treatment recommendation is another critical feature of advanced healthcare AI systems. By analyzing individual patient characteristics, genetic information, lifestyle factors, and treatment history, these systems can suggest tailored treatment approaches that are more likely to be effective for specific patients. This moves beyond one-size-fits-all medicine toward truly personalized care that considers each patient's unique circumstances and needs.
Operational optimization capabilities help healthcare organizations improve efficiency and reduce costs. AI systems can optimize scheduling, resource allocation, inventory management, and workflow processes, leading to better patient flow and reduced wait times. These operational improvements not only enhance efficiency but also contribute to better patient experiences and outcomes by ensuring that resources are available when and where they're needed most.
Remote patient monitoring and telehealth support have become increasingly important features, especially in the context of the COVID-19 pandemic and beyond. AI-powered systems can analyze data from wearable devices, home monitoring equipment, and virtual consultations to track patient health status, identify concerning trends, and facilitate timely interventions. This enables more continuous and comprehensive care outside traditional clinical settings.
Pros and Cons of Leveraging AI in Healthcare
The integration of AI into healthcare offers numerous potential benefits, but also presents significant challenges and risks that must be carefully managed. Understanding both sides of this equation is essential for making informed decisions about AI adoption and implementation.
Advantages of AI in Healthcare
Improved diagnostic accuracy stands as one of the most significant benefits of healthcare AI. AI algorithms can analyze complex patterns in medical data that may be difficult for humans to detect consistently. For example, in medical imaging, AI systems have demonstrated the ability to identify subtle signs of disease that might be missed by human radiologists, leading to earlier detection and treatment of conditions like cancer, cardiovascular disease, and neurological disorders.
Enhanced efficiency and productivity represent another major advantage. AI can automate routine tasks such as documentation, data entry, and administrative processes, freeing healthcare professionals to focus on more complex and value-added activities. This not only improves workflow efficiency but also helps address workforce shortages and burnout by reducing administrative burden.
Personalized medicine capabilities allow for treatments tailored to individual patient characteristics, leading to better outcomes and reduced side effects. By analyzing genetic information, lifestyle factors, and treatment history, AI systems can identify the most effective interventions for specific patients, moving beyond the one-size-fits-all approach that has traditionally dominated medicine.
Predictive analytics enable proactive interventions by identifying patients at risk of developing complications or requiring hospitalization. This allows healthcare providers to intervene early, potentially preventing adverse outcomes and reducing healthcare costs. Predictive models can also help optimize resource allocation and planning, ensuring that healthcare organizations are prepared to meet patient needs effectively.
Accessibility improvements represent another significant benefit, particularly through telehealth and remote monitoring applications. AI-powered tools can extend healthcare expertise to underserved areas, provide continuous monitoring for chronic conditions, and offer convenient access to care for patients who might otherwise face barriers to traditional healthcare services.
Challenges and Risks of AI in Healthcare
Data privacy and security concerns represent one of the most significant challenges in healthcare AI. The sensitive nature of health information requires robust protections, and the extensive data collection needed for AI training and operation creates potential vulnerabilities. Ensuring compliance with regulations like HIPAA while maintaining the data access needed for effective AI operation presents an ongoing challenge.
Algorithmic bias and fairness issues pose serious risks if not properly addressed. AI systems trained on biased or unrepresentative data may perpetuate or even amplify existing healthcare disparities. Ensuring that AI tools work equitably across different demographic groups requires careful attention to data collection, algorithm design, and validation processes.
Implementation costs and resource requirements can be substantial, particularly for smaller healthcare organizations. Beyond the initial investment in technology, AI implementation requires ongoing maintenance, updates, and staff training. These costs must be carefully weighed against expected benefits, and organizations must ensure they have the infrastructure and expertise to support AI systems effectively.
Integration with existing workflows presents practical challenges that can undermine the effectiveness of even the most sophisticated AI tools. If AI systems disrupt clinical workflows or create additional burdens for healthcare professionals, they may not be adopted or used effectively. Successful integration requires thoughtful design that aligns with how clinicians actually work and adds genuine value to their practice.
Regulatory and liability considerations create additional complexity for healthcare AI. The regulatory landscape is still evolving, and questions about accountability when AI systems contribute to clinical decisions remain unresolved. Navigating these uncertainties while ensuring patient safety and regulatory compliance requires careful attention and ongoing adaptation as the field develops.
Frequently Asked Questions
How does AI improve diagnostic accuracy in healthcare?
AI improves diagnostic accuracy through several mechanisms. First, AI algorithms can analyze vast amounts of data—including medical images, lab results, and clinical notes—to identify subtle patterns that might be difficult for humans to detect consistently. These systems don't suffer from fatigue, distraction, or cognitive biases in the same way human clinicians might, leading to more consistent performance. Second, AI can integrate information from multiple sources to provide a more comprehensive assessment than might be possible through human analysis alone. For example, an AI system might combine imaging data with genetic information and clinical history to generate a more accurate diagnosis. Third, AI systems can be trained on massive datasets that represent diverse patient populations and disease presentations, allowing them to recognize rare or atypical cases that individual clinicians might encounter only infrequently. However, it's important to note that AI should augment, not replace, human expertise—the most effective approach typically involves collaboration between AI systems and healthcare professionals.
What are the biggest ethical concerns with AI in healthcare?
The ethical concerns surrounding AI in healthcare are multifaceted and significant. Algorithmic bias represents one of the most pressing issues—if AI systems are trained on biased or unrepresentative data, they may perpetuate or even amplify existing healthcare disparities across different demographic groups. Privacy and data security concerns are equally important, as healthcare AI requires access to sensitive patient information, creating potential vulnerabilities. Transparency and explainability present another major ethical challenge—many AI systems operate as "black boxes" whose decision-making processes are difficult to understand or explain, which can undermine trust and accountability. Informed consent becomes more complex when AI is involved in clinical decision-making, as patients may not fully understand how these systems work or what role they play in their care. Finally, there are concerns about the potential dehumanization of healthcare and the erosion of the patient-clinician relationship if AI systems are implemented without careful attention to preserving human connection and empathy in medical care.
How can healthcare organizations prepare for AI implementation?
Healthcare organizations can take several steps to prepare for successful AI implementation. First, they should develop a clear AI strategy aligned with their clinical priorities and organizational goals, identifying specific problems where AI might provide meaningful solutions rather than pursuing technology for its own sake. Second, organizations need to assess and improve their data infrastructure, ensuring they have systems in place to collect, store, and manage high-quality data in a secure and compliant manner. Third, investing in staff education and change management is crucial—healthcare professionals need to understand how AI tools work, what benefits they offer, and how to integrate them effectively into their workflows. Fourth, organizations should establish governance frameworks for AI oversight, including processes for evaluating AI tools, monitoring their performance, and addressing any issues that arise. Fifth, pilot programs and phased implementations can help organizations learn and adapt before scaling AI solutions across the entire organization. Finally, fostering partnerships with technology developers, academic institutions, and other healthcare organizations can provide valuable expertise and resources for successful AI adoption.
What types of healthcare data are most valuable for AI applications?
Different types of healthcare data offer unique value for AI applications, with the most powerful insights often coming from integrating multiple data types. Structured clinical data from electronic health records—including diagnoses, medications, lab results, and vital signs—provide essential information for many AI applications, particularly those focused on predictive analytics and clinical decision support. Medical imaging data (X-rays, CT scans, MRIs, etc.) are invaluable for AI systems specializing in image analysis and diagnostic assistance. Genomic and molecular data enable personalized medicine applications by revealing individual variations that influence disease risk and treatment response. Real-world data from wearable devices and remote monitoring tools offer continuous, longitudinal information about patient health status outside clinical settings. Unstructured data from clinical notes, research literature, and patient-generated content can be analyzed using natural language processing to extract valuable insights that might not be captured in structured formats. The integration of these diverse data types often produces the most comprehensive and accurate AI systems, though it also presents significant technical and privacy challenges.
How does AI handle the variability and uncertainty inherent in medical practice?
AI systems handle medical variability and uncertainty through several advanced techniques. Probabilistic modeling allows AI systems to express predictions as probabilities rather than certainties, reflecting the inherent uncertainty in medical decision-making. Bayesian approaches explicitly incorporate prior knowledge and update beliefs as new evidence becomes available, similar to how clinicians adjust their thinking based on additional information. Ensemble methods combine multiple models to produce more robust predictions that are less vulnerable to the limitations of any single approach. Uncertainty quantification techniques help AI systems recognize when they encounter situations where their predictions are less reliable, allowing them to express appropriate caution or defer to human experts. Transfer learning enables AI systems to apply knowledge gained from one domain to another, helping them handle rare conditions or unusual presentations that may not be well-represented in training data. Finally, many AI systems are designed to work collaboratively with human clinicians, providing decision support rather than autonomous decision-making, which allows human expertise to handle edge cases and uncertainties that challenge algorithmic approaches.
Related Questions: Exploring Further Implications
How does AI impact medical education and training?
AI is transforming medical education by providing personalized learning experiences, simulating complex clinical scenarios, and offering real-time feedback to trainees.
What role does AI play in drug discovery and development?
AI accelerates drug discovery by predicting molecular interactions, identifying potential drug candidates, and optimizing clinical trial designs.
How are regulatory agencies adapting to healthcare AI?
Regulatory agencies are developing new frameworks for evaluating AI-based medical devices while balancing innovation with patient safety requirements.
What are the implications of AI for healthcare costs and economics?
AI has potential to reduce costs through improved efficiency and prevention but requires significant upfront investment and ongoing maintenance expenses.
Relevant AI & Tech Trends articles
Stay up-to-date with the latest insights, tools, and innovations shaping the future of AI and technology.

AI Tattoo Design: Creating Empowering Art with Affirmations
Published on: September 10, 2025

TWICE's 'Imaginary Friends': A Deep Dive into the Revolutionary K-Pop Masterpiece
Published on: September 10, 2025